Healthcare interoperability initiatives have been going on for quite some time now, with varying degrees of success. While some interoperability efforts have been successful and are expanding reach, others have shut down completely.
So what is the state of healthcare interoperability in 2019? New England HIMSS examined this topic in its annual HIE Conference—a day devoted to exploring some of the issues around interoperability and health exchanges. Let’s examine some of the takeaways from the event.
Healthcare interoperability: a definition
According to HIMSS:
“Interoperability is the ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner, within and across organizational, regional, and national boundaries, to provide timely and seamless portability of information and optimize the health of individuals and populations globally.”
Bruno Nardone of NextGen Healthcare started the program by talking about the interoperability continuum. It starts with the patient-provider relationship and an encounter being documented in the patient’s medical record. It then moves up to an entire practice, an enterprise, and eventually to a regional health information exchange (HIE). These HIEs allow healthcare institutions to share patient information electronically, despite different technology systems in place.

There are various regulatory and legislative initiatives—such as the 21st Century Cures Act and 42 CFR – that address interoperability. However, these initiatives dictate minimum sharing requirements. It’s up to organizations to decide their strategic initiatives and how interoperability figures into that. For many, that means figuring out how interoperability factors into the Quadruple Aim.
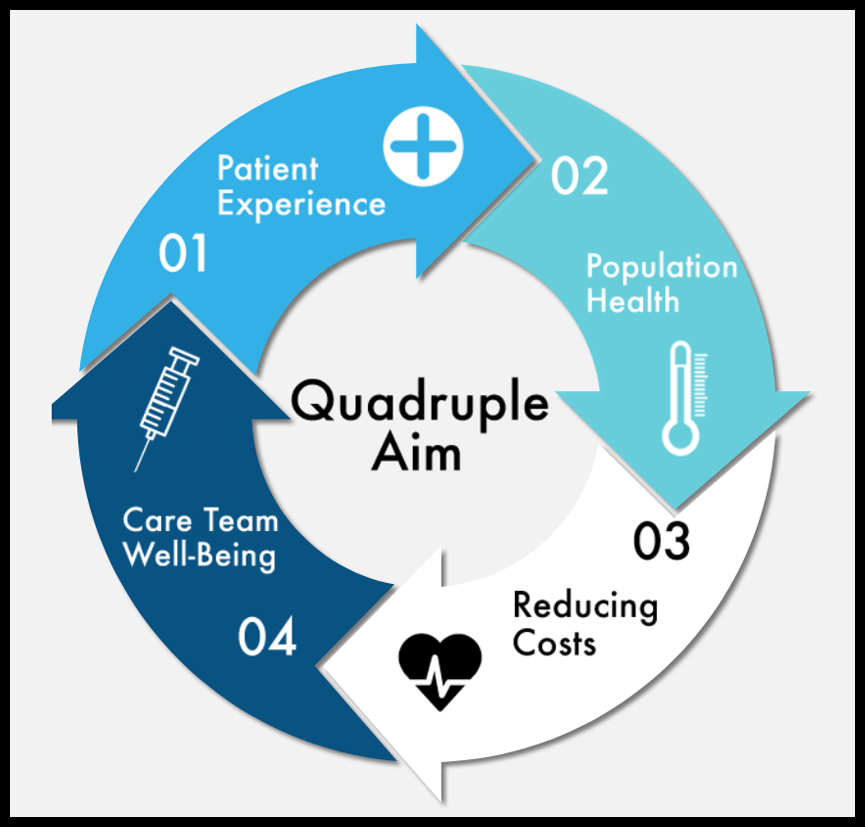
Source: UAMS, https://ipe.uams.edu/about-us/ihi-triple-aim/
Successful examples of HIEs
Daniel Porreca of HEALTHeLINK in Western New York and Laura McCrary of KONZA in Kansas spoke at the event about their successful HIEs.
Porreca discussed some of HEALTHeLINK’s successes, including:
- Significant improvements in tracking, treating, and reducing the spread of STDs
- Reduction of unnecessary CT scans in the hospital setting
- A 52% reduction in lab testing and a 47% reduction in radiology exams in the emergency department
- 18- to 40-minute reduction in patient cycle time due to workflow efficiencies
In short, Porreca explained that greater information sharing between healthcare organizations leads to reduced tests and greater workflow and cost efficiencies – benefiting both the patient and the healthcare provider.
McCrary talked about the successes she has seen at KONZA, but also talked about some of the failures of other HIEs. She said that many EHR vendors are taking over the role of sharing data—but in many cases, they don’t do it as effectively, as they are not integrating data from the broad variety of sources that should be integrated, including hospitals, doctors’ offices, pharmacies, urgent care centers, and so on. Unfortunately, though, many HIEs disbanded because of the EHR efforts.
McCrary maintains that the value of HIEs is in the data they hold. HIEs have been collecting data for years now, and they are uniquely positioned to bring together and make available a large part of healthcare data.
Healthcare interoperability in action
As part of the HIE Day program, John Goldie and Rebecca Mishuris talked about Boston Medical Center’s need for an HIE, given its accountable care organization (ACO). The health system currently has 4 Medicaid ACO joint ventures, 6 hospitals, and 18 community health centers.
In order to drive performance in the Medicaid ACO program, it needs access to lots of data. This data helps it to coordinate care better, see how it is doing on quality measures, and better manage its total cost of care. That requires a complex integration of multiple data sources, such as multiple EHRs, claims data, care management data, and more. The organization is also looking into how to better integrate social determinants of health (SDOH) so it can segment its patients by SDOH factor.
Conclusion
Many in the industry would hope that healthcare interoperability would be further along than it is right now. The potential for cost savings and improved patient outcomes that comes with freely shared data is so high. While there are legislative and regulatory initiatives that are mandating some data sharing, ultimately it is up to healthcare organizations and technology companies to determine what is of strategic value. Events such as this one prove useful to see what’s successful in healthcare interoperability and what needs to be improved upon.
Related articles
- Promoting Diversity and Inclusion in Healthcare
- Celebrating Women in Healthcare Leadership
- The Future of Healthcare: What Can We Expect by 2025?
- Solving Hospital CEOs’ Pressing Challenges With Analytics - April 15, 2024
- Navigating the Wellness Wave: Wine & Spirits Data Strategy - April 9, 2024
- Takeaways from HIMSS24 - March 26, 2024