Propelled by recent technological breakthroughs like ChatGPT and Bard, artificial intelligence (AI) has catapulted into the mainstream as an indispensable digital assistant. On the heels of its success, AI is now making swift inroads across industries, with healthcare being no exception. AI seems poised to revolutionize the field with the promise of addressing pressing challenges in the healthcare industry, such as rising costs, clinician burnout, and workforce shortages.
However, while AI presents immense potential, healthcare institutions must approach its adoption responsibly, considering both the advantages and potential pitfalls. AI may be gaining steam, but prudent evaluation of benefits and risks remains vital as healthcare explores integrating this emerging technology into critical workflows.
Applications of AI in healthcare
AI has a multitude of potential applications that could transform healthcare. Diagnostic procedures, for instance, are seeing a paradigm shift with AI imaging algorithms, which can detect anomalies such as lung nodules and diagnose conditions such as diabetic retinopathy with higher accuracy than many clinicians. Natural language processing models have ushered in a new era where patient-doctor conversations can be converted into clinical notes automatically. Furthermore, AI-driven chatbots have started providing patients with personalized education and follow-ups, helping to bridge care gaps.
The potential of AI doesn’t end there. AI-powered predictive analytics can flag patients at potential risk of disease or hospital readmission, facilitating early and timely interventions. Operational challenges, such as surgery scheduling, and administrative tasks, such as medical billing, can be streamlined using AI, leading to smoother patient experiences and reduced wait times. The crux lies in leveraging AI’s ability to discern patterns in data, augmenting the capabilities of healthcare professionals and offering them more bandwidth for patient care.
Yet, for AI to truly flourish in healthcare, a robust digital data infrastructure is imperative. Healthcare data is often scattered across siloed systems, plagued by issues of compatibility, completeness, and security. Establishing strong data management, developing an analytics strategy, and instituting proper governance acts as a critical foundation for AI to build upon. With comprehensive, trustworthy data as a baseline, hospitals can strategically identify high-impact AI opportunities.
The need for responsible AI adoption
AI’s growing presence in healthcare necessitates an ethical and transparent approach to its implementation. As stewards of protected health information (PHI), maintaining patient privacy and complying with regulations such as HIPAA must be top priorities. Additionally, ensuring that AI models are free from biases, transparent in their functioning, and meticulously validated for accuracy is essential to fostering trust.
Furthermore, clinicians should be equipped with training to use AI tools and interpret their output effectively. For instance, while AI can identify anomalies in medical images with precision, the broader clinical context remains a human skill. AI should thus complement, not replace, clinician judgment and expertise. Moreover, hospitals need to navigate the murky waters of AI ethics, considering questions around accountability, consent, and patient awareness regarding AI’s role in their care. If AI makes a faulty recommendation that ultimately harms a patient, who is liable? And should patients be informed when an AI is involved in their care? Thoughtful policies are needed.
A strategic approach: lead or lag?
With the immense promise of AI to support physician productivity, alleviate burnout, and improve patient outcomes, the case for adopting AI in healthcare is compelling. However, integrating AI into clinical workflows is not a simple decision—it requires careful strategy. When weighing AI adoption, hospitals must tread carefully and evaluate the costs, benefits, and potential risks. There should be adequate training and appropriate safeguards in place before implementation. AI’s impact should be continuously monitored and iteratively improved through cycles of deployment, feedback, and refinement.
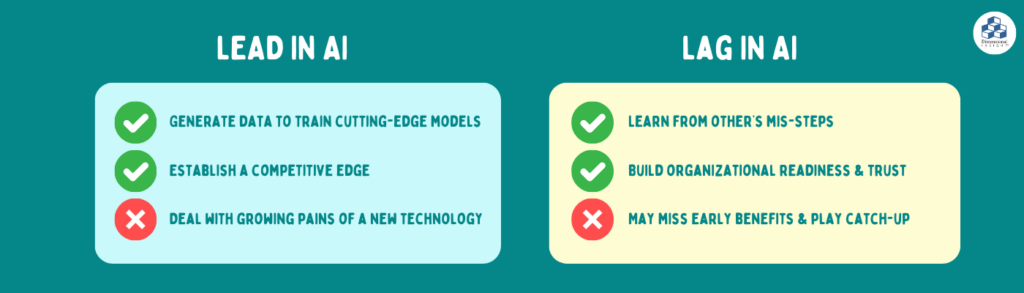
Hospitals that lead in adopting AI take a calculated risk, accepting the growing pains of an emerging technology. However, first movers could also realize advantages such as establishing a competitive edge, attracting top talent, generating data to train cutting-edge models, and collaborating with partners to shape AI guidelines. Conversely, hospitals that lag can learn from others’ missteps and implement more mature AI, but miss out on potential early benefits while playing catch-up. A “wait and see” approach also allows time to build organizational readiness and clinician trust in AI.
There are merits to both approaches. The key is weighing factors such as risk tolerance, resources, clinician buy-in, and goals to make a context-specific plan, such as piloting AI in low-risk workflows before expanding. No approach is inherently right or wrong; rather, the key is rolling out AI in a thoughtful way that aligns with organizational goals and culture.
Looking Ahead
AI’s potential in healthcare is vast, promising improved patient care, reduced costs, and operational efficiency. However, its adoption should be strategic and measured. The future of healthcare with AI looks bright, but a judicious approach that melds optimism with caution will ensure that healthcare remains effective, equitable, and safe. With responsible implementation, AI can usher in a new era of healthcare that empowers both patients and providers.
- Why We’re Best in KLAS—Again! - February 7, 2024
- Building a Greener Healthcare System with Data Analytics - January 22, 2024
- Hospital Finance Predictions for 2024 - January 8, 2024