 We hear a lot about the promise of healthcare analytics, but what is actually being done on the front lines that is making a difference right now? This is the central issue I’m examining in this blog series on “Analytics in the Real World of Healthcare.”
We hear a lot about the promise of healthcare analytics, but what is actually being done on the front lines that is making a difference right now? This is the central issue I’m examining in this blog series on “Analytics in the Real World of Healthcare.”
In the first post of this series, I referred to an example of an organization-wide initiative to “move the needle” on important measures associated with cost and quality. This second post looks at analytics from a different perspective: integrating information from clinical processes directly into a closed-loop analytics system to improve direct patient care. Here we’ll take a look at how analytics is being applied to reduce post-surgery mortality rates.
Tweet: Analytics in the Real World of Healthcare: Improving Surgical Outcomes
The topic for this post was inspired by a presentation given by Dr. Wolf Stapelfeldt during the Clinical & Business Intelligence (C&BI) Symposium that preceded HIMSS 2015 this past April. What made this presentation particularly intriguing was Dr. Stapelfeldt’s deep expertise in both the medical and analytics domains. He is the chair of the Department of Anesthesiology and Critical Care Medicine at Saint Louis University Medical Center. He also is a founding member of the HIMSS C&BI Community and has strong credentials in research methods and statistical analysis. His presentation summarized the result of several years of research and provided a glimpse into the possibilities — and likely direction — of incorporating analytics directly into the practice of medicine.
The presentation included more than 200 slides so I’ll stick with the highlights and key takeaways.
Integrating Closed-Loop Analytics into Patient Care to Produce Real Results
The presentation’s underlying message was that, as a result of electronic health record (EHR) technologies, there are now opportunities to integrate closed-loop analytics systems directly into patient care processes. The illustration (Figure 1, below, from Dr. Stapelfeldt’s presentation) shows how operational processes (represented by the loop on the left) are complementary to corresponding analytical processes (the loop on the right) in that they produce information that can be used immediately for decision support as well as contribute to an ever growing body of information that can be used to continuously refine the operational processes. In this context, operational processes include front line medical care.
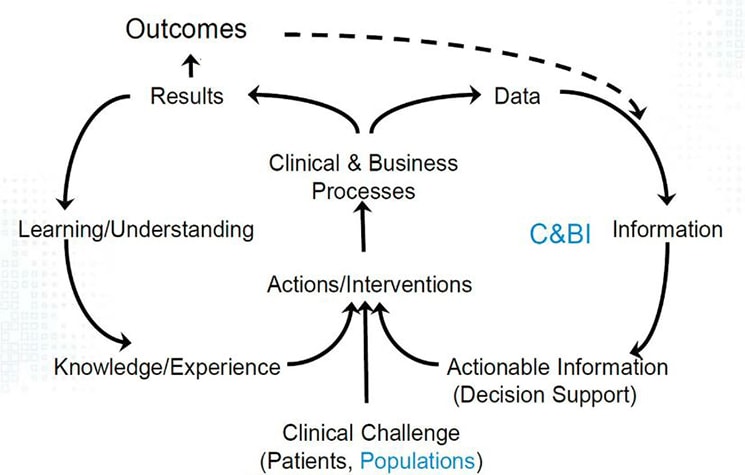
Figure 1
Source: The SLUScore™: A Novel Method to Quantify the Adverse Impact of Intraoperative Hypotension on Patient Outcome Following Non-Cardiac Surgery
Dr. Stapelfeldt advised that for this approach to be successful, you need to be willing to change your perspective and approach as the environment changes. He used an analogy from the trucking and logistics industry to make the point. In the era before the interstate highway system, the best trucking route between Chicago and Los Angeles was the shortest: Route 66. The time required to make the trip was influenced by a combination of the overall distance, speed limits and stop lights. The advent of superhighways provided alternative routes that increased the distance, yet reduced travel time. As truckers were willing to consider longer alternatives, they discovered routes that were ultimately more efficient. Translating this into the world of healthcare, the availability of more, better and timelier information opens up a whole new world of possibilities for improving care, both at the individual and population levels.
Focusing on Outcomes Should Be Highest Priority
The main scenario focused on a research initiative to identify opportunities for significantly improving outcomes from surgical procedures. This emphasis on outcomes was not only central to the research but also represents an important trend in healthcare analytics. Dr. Stapelfeldt suggested that the highest priority for C&BI should be to focus on meaningful outcomes related to conditions that cause suffering, are expensive to treat and tend to get worse. However, selecting the most appropriate outcome measurements is an exercise in itself. There are many relevant options to choose from, including cost, readmissions, length or stay, mortality and so on.
So how did his team decide what to focus on? Research shows that on average, more than 2% of patients undergoing non-cardiac surgery die within 30 days of the procedure. Not only that, but the rate of post-surgical mortality in the U.S. is high compared with other countries and it is on the rise. Given the severity of this outcome and the negative trend, his research team opted to focus on this measure for its initiative.
A population of more than 116,000 patients undergoing surgical procedures at Saint Louis University Medical Center, Cleveland Clinic and Vanderbilt University Medical Center provided a rich data set for the research. This also was ideal for applications of descriptive, predictive, and prescriptive analytics alike. Researchers used logistic regression techniques to identify the variables that influenced the outcome measures most significantly. What bubbled to the top was the observation that prolonged exposure to hypotension (low blood pressure) during surgery was a strong predictor of 30 day mortality. However, the patterns around specific thresholds and time of exposure took plenty of heads down work to tease out. The presentation has more details on this as well as some very interesting approaches to visualizing relationships among three variables.
The evidence from the research yielded a matrix that represents the relationships between hypotension thresholds, time of exposure and the mortality outcome measure. The challenge lies in translating this clinical evidence into something that could be practically used on the front lines of medicine. And the solution to this problem was one of the most innovative aspects of the initiative: a fairly simple measure that counted the number of times the thresholds were reached during surgery. This measure, called the SLUScore (SLU for Saint Louis University), showed a strong correlation with the outcome measure. Surgical patients in the research population with a SLUScore greater than zero were twice as likely to succumb within 30 days as those with a SLUScore of zero. (Figure 2, below, from Stapelfeldt’s presentation)
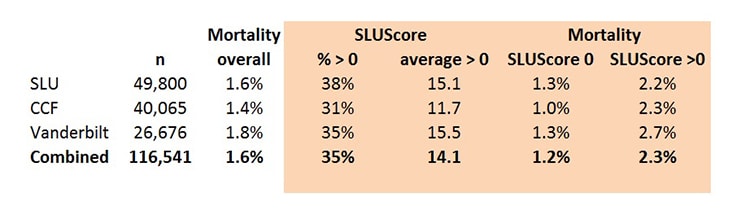
Figure 2
Source: The SLUScore™: A Novel Method to Quantify the Adverse Impact of Intraoperative Hypotension on Patient Outcome Following Non-Cardiac Surgery
Turning Analytical Observations into Change in the OR
This is the point where the theory moves into practice. The evidence from the research was incorporated into a decision support system, called “Advanced Clinical Guidance – Anesthesia” which monitors blood pressure and other vital signs during a surgical procedure and continuously re-computes the SLUScore. The system consists of components that 1) collect physiologic data, 2) process it through a knowledge base that contains clinical evidence, and 3) present “actionable” information via alerts in a decision support interface to the surgical team throughout the procedure. These alerts provide opportunities to intervene both during the procedure as well as the during the recovery period and post hospitalization care.
The information captured by the decision support system contributes to an overall dataset that can be used to further refine the SLUScore and also identify other potential contributors to the mortality and other outcome measures. Incidentally, the research also showed a strong correlation between the SLUScores and other outcome measures based on cost, length of stay, and readmissions.
All in all, this was a pretty impressive example of applying analytics in a very practical way that demonstrates the potential for real impact on important outcomes. But this type of closed loop decision support system has only become possible recently as the adoption of EHR technology has increased. Think of the additional possibilities as both access to data and knowledge of how to work with it increases!
Ready for a test drive of our healthcare analytics software?
- Practical Analysis: The Next Chapter - May 21, 2020
- Exploratory Data Analysis Part 2: Helping You Make Better Decisions - October 11, 2019
- Practical Analysis: Understanding Visualization Concepts - September 19, 2019



