Data governance used to be something healthcare organizations talked about but rarely operationalized. Today, it’s become the backbone of trustworthy analytics, AI readiness, and confident decision-making. As data becomes more complex and more central to care delivery, governance is no longer optional—it’s the only way hospitals and health systems can ensure their data is accurate, secure, and interpreted consistently across clinical, financial, and operational domains.
In our work with healthcare organizations of all sizes, one theme shows up again and again: analytics doesn’t succeed because of tools alone. It succeeds because the organization has a governance framework that creates clarity, accountability, and trust.
Here’s how to build a healthcare data governance program that actually works—one that improves data quality, strengthens compliance, and accelerates better decisions.
Start With Outcomes, Not Policies
The biggest mistake organizations make is treating governance as a documentation exercise. Governance isn’t about creating binders of policies—it’s about enabling better outcomes.
Before you assemble a committee or define roles, identify the 3–5 goals governance must support. These might include:
- Reducing report disputes between departments
- Standardizing KPI definitions (LOS, readmissions, encounters, charges)
- Improving regulatory reporting accuracy
- Strengthening data quality for AI and predictive models
- Shortening the time from question → insight → action
When governance is tied directly to outcomes, adoption increases, decisions move faster, and your analytics program becomes far more sustainable.
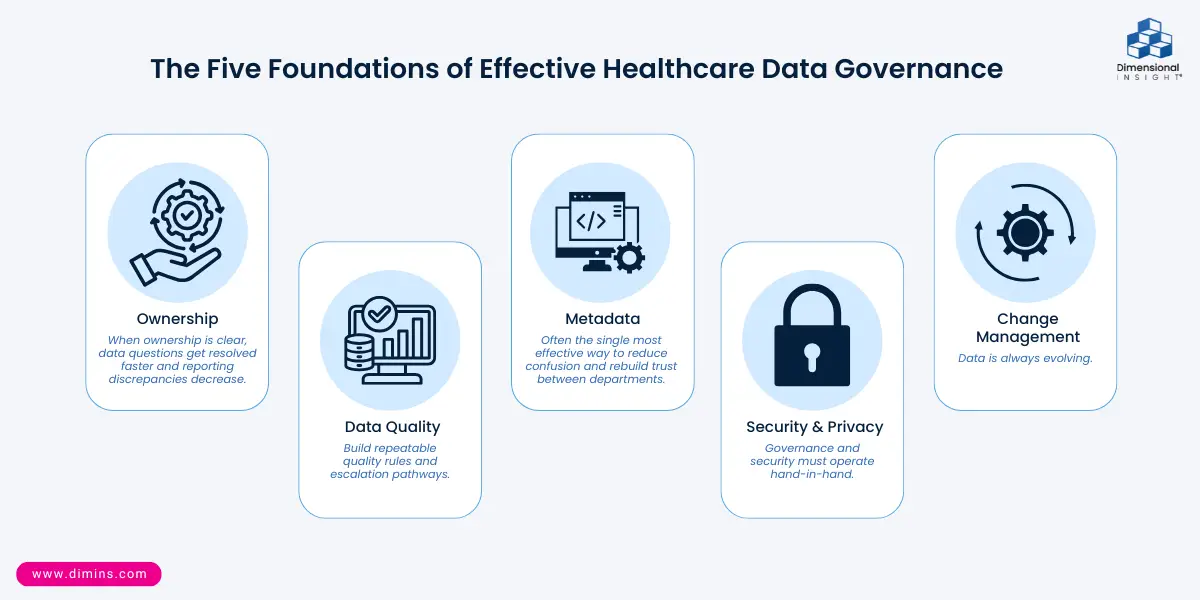
The Five Foundations of Effective Healthcare Data Governance
Based on work with leading hospitals and health systems, five foundational elements consistently determine whether governance succeeds:
- Ownership: Assign accountable data owners and stewards for each domain—clinical, financial, operational. When ownership is clear, data questions get resolved faster and reporting discrepancies decrease.
- Data Quality: Define how data will be validated, profiled, reconciled, and monitored over time. Build repeatable quality rules and escalation pathways.
- Metadata: Maintain a shared data dictionary and KPI catalog so every user interprets metrics the same way. This is often the single most effective way to reduce confusion and rebuild trust between departments.
- Security & Privacy: Ensure role-based access, audit trails, HIPAA compliance, and alignment with frameworks such as HITRUST and NIST. Governance and security must operate hand-in-hand.
- Change Management: Data is always evolving. Governance teams must communicate definition changes, new data sources, refreshed quality rules, and system updates so users never feel “surprised” by their dashboards.
When these five elements are in place, your analytics program becomes more accurate, faster to maintain, and dramatically more trusted.
Build a Governance Structure That’s Lightweight—but Clear
Healthcare teams are stretched thin. The key is to create structure without bureaucracy.
At a minimum, define four essential roles:
- Data Owners – accountable for strategic decisions in each domain
- Data Stewards – responsible for definitions, lineage, quality, and documentation
- Data Custodians / IT – enabling access, security, and technical implementation
- Governance Council – cross-functional decision-making body
Use a simple RACI (Responsible, Accountable, Consulted, Informed) to clarify who decides what. Meetings should be short, structured, and focused on high-impact items, not theoretical discussions.
Standardize Definitions to Eliminate Confusion
Few things erode trust faster than two teams presenting two different numbers for the same KPI.
To establish consistency:
- Start with high-value metrics with known variation (readmissions, LOS, ED throughput, encounters).
- Document definitions, source logic, lineage, calculations, and update cycles.
- Align definitions to industry standards like HL7, FHIR, CMS quality measures, or state reporting requirements.
- Store everything in your metadata layer so it’s accessible to every stakeholder.
When clinicians and executives have a single source of truth for core metrics, data becomes a strategic asset rather than a point of debate.
Create a Repeatable Data Quality Lifecycle
Great analytics cannot exist without great data quality. Build a continuous improvement loop:
Profile → Detect → Prioritize → Resolve → Monitor → Communicate
Focus quality efforts on the domains that matter most, such as:
- Patient identity management
- Clinical documentation integrity
- Charge capture accuracy
- Coding completeness
- ED and surgical workflow data
Quality shouldn’t be reactive. Your governance framework should prevent problems before they affect operations, reporting, or patient care.
Connect Governance With Privacy, Security & Regulatory Compliance
Governance, security, and privacy must be integrated, not siloed. Without this alignment:
- Access controls become inconsistent
- Audit trails break down
- PHI risks increase
- Definitions drift over time
Make sure your governance program reinforces:
- HIPAA requirements
- HITRUST control frameworks
- NIST security standards
- Organizational retention and access policies
This ensures your analytics and AI environment remains compliant, auditable, and safe.
Governance Is the Foundation of AI Readiness
As hospitals explore predictive analytics, natural-language interfaces, and LLM-enabled copilots, governance becomes even more essential.
Without strong definitions, lineage, and quality rules:
- AI features become unexplainable
- Predictions become unreliable
- Model drift accelerates
- Privacy risks multiply
Governance ensures that:
- Every model input is defined and validated
- Lineage is traceable
- Data refresh cycles are documented
- Outputs can be explained in plain language
Healthcare leaders increasingly recognize that trustworthy AI starts with trustworthy data—and trustworthy data starts with governance.
Operationalizing Governance: Your Month-to-Month Rhythm
The most successful governance programs adopt a simple, repeatable operating cadence:
- Monthly Governance Committee Meetings: Review definitions, approve changes, evaluate open data quality issues
- Quarterly Data Quality Reviews: Evaluate domain-level quality metrics and identify improvement areas
- Definition Update Cycles: Update KPI logic, metadata entries, lineage documentation
- Governance Dashboards: Track quality, ownership assignments, open issues, SLA compliance, and adoption
Governance isn’t a one-time project—it’s a continuous, lightweight discipline.
A Simple 90-Day Roadmap to Get Started
If you’re building or revamping a governance program, start small and simple:
Days 1–30: Establish the Foundation
- Identify priority domains
- Assign owners and stewards
- Inventory definitions and data sources
Days 31–60: Build Your Structure
- Create your governance council
- Draft your initial data dictionary
- Implement basic quality rules
Days 61–90: Operationalize
- Launch monthly committees
- Begin monitoring quality KPIs
- Document lineage for high-value measures
Small wins build momentum quickly—and help your organization see immediate value.
Conclusion: Governance Isn’t About Control—It’s About Confidence
Healthcare organizations don’t need more dashboards. They need data they can trust.
A strong governance program:
- Improves data quality
- Reduces rework and disputes
- Enhances compliance
- Accelerates decision-making
- Strengthens AI readiness
- Builds lasting trust across the organization
The most successful healthcare analytics programs—whether focused on operations, clinical quality, revenue, or innovation—all share the same foundation: governance that works.
If you’d like help assessing your current governance maturity or building a roadmap tailored to your organization, our team is here to help.

- How to Build a Healthcare Data Governance Program That Actually Works - December 23, 2025
- What the 2025 Gartner Peer Insights Voice of the Customer Report Tells Us About Analytics and Customer Experience - December 16, 2025
- How Healthcare Organizations Use Analytics to Improve Outcomes - December 9, 2025