The COVID-19 pandemic has officially been in our lives for a full year. Although it’s given us bad news time and time and again, three different vaccines have begun their distribution nationwide, which gives many individuals hope for a COVID-free life in the near future. However, while the United States is trying to vaccinate people as quickly and efficiently as possible, distribution stages vary state by state. Unfortunately, there is major healthcare inequity among certain populations, creating a barrier between receiving a vaccine and not being able to. However, Federally Qualified Health Centers, otherwise known as FQHCs, are helping to improve this issue. Here’s how:
The issue
The main purpose of FQHCs is to provide “safety net” primary care providers and other health resources for vulnerable populations across the nation, all in one place. These health centers operate on a not-for-profit basis and their patients often fall under vulnerable populations such as low-income, little or no commercial insurance, several comorbidities, and oftentimes, these individuals are people of color. Because of these disparities, FQHC patients usually can’t afford good health insurance which is needed to ensure an individual’s good health as well as their family members. When met with this challenge, many patients end up going into medical debt when they do end up needing to seek healthcare. It’s obvious that no one would want to go into medical debt, so what happens when a low-income individual is faced with the choice of receiving medical attention for an unreasonably high price or risking having their health get worse for the price of nothing? Unfortunately, most people in this situation will choose the latter, which snowball-effects into putting vulnerable populations at higher risk for contracting diseases such as COVID-19, which can even lower their expectancy rate over time—simply due to the color of their skin or the amount of money they earn for themselves or their families.

What FQHCs are doing to help healthcare inequity during vaccine rollout and the challenges that come with doing so
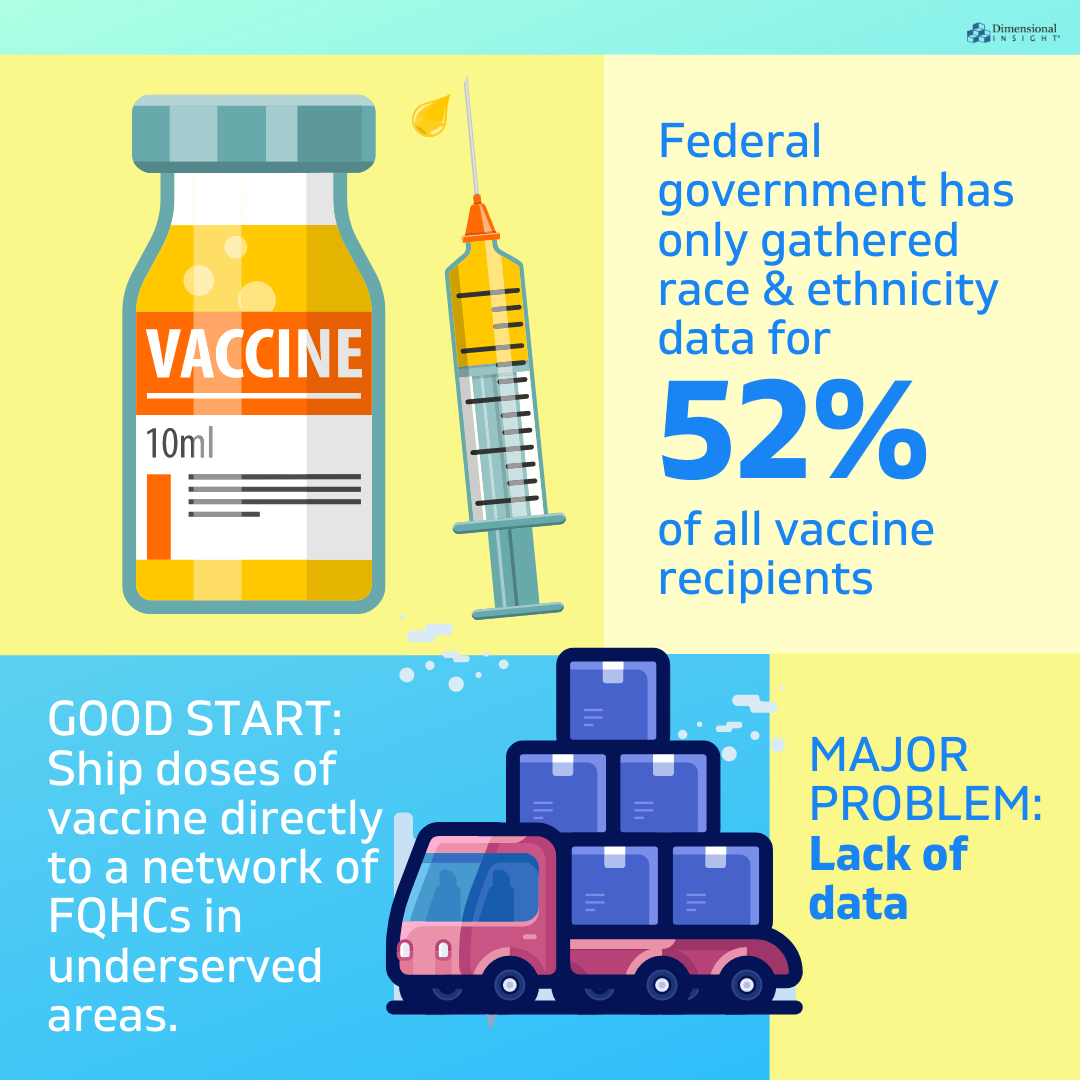
With a new president who claims that racial equity will be at the core of his administration’s response to the pandemic, White House officials recently announced a program to ship doses of vaccine directly to a network of FQHCs in underserved areas. These types of programs are a great start, but there are a few barriers that make it difficult for positive results to be seen—one of the barriers being the lack of data.
According to the CDC, the federal government has only gathered race and ethnicity data for 52 percent of all vaccine recipients, which in the long run is definitely a start but also nothing to celebrate quite yet. The New York Times notes that public health experts agree that delivering vaccines directly to underserved communities is helpful, but that the “absence of comprehensive data makes it impossible to know whether vaccine distribution is truly equitable, and how to correct disparities.” When the vaccine rollout is on a first-come, first-serve basis, the privileged will often get access first, despite initiatives that may be developing to prevent such an occurrence from happening.
“The race and ethnicity data is important because we know who’s bearing the brunt of the pandemic, so there is a fairness and an empathy issue. But there is also a disease control issue. If those are the groups most likely to get affected and die, those are the groups we need to make sure we are reaching with vaccine,” emphasizes Dr. Marcus Plescia, chief medical officer of the Association of State and Territorial Health Officials.
So why the lack of data? A few reasons are that not all states allow the release of information such as ethnicity, and patients aren’t required to fill that information in when they register, which makes the collected data inconsistent. Arkansas is one example of a state that has a lack of data when it comes to helpful information that could potentially close the gap of racial and minority health inequity, as it’s missing about one third of its race and ethnicity data from those who have been vaccinated, despite officials trying to obtain the data.
Although the lack of data is concerning for some health experts, FQHCs are continuing to do their best with the data they do have in order to help combat the issue. According to Kaiser Family Foundation, 54% of people who received their first dose of the COVID-19 vaccine from an FQHC were people of color, including 26% who were Hispanic and 12% who were Black, which are higher than the shares of nationwide vaccinations. “The CDC data shows that 9% of the people receiving one more dose of vaccine as of March 7, 2021 were Hispanic and 7% were Black. The shares of health center vaccinations received by people of color increased in more recent weeks compared to vaccinations in January 2021.”
What this means for potential lasting change in the healthcare system
Healthcare inequity has been in existence from the very beginning and this unpredictable pandemic was hopefully the extra little push it took for the issue to really come into light and be taken seriously. As discussed throughout the article, FQHCs have already been serving the most vulnerable populations in the United States, including those in the BIPOC, low-income, and immigrant communities as that’s the core purpose and mission of such health centers. With the vaccine rollout, these centers are doing a better job at capturing racial and ethnic data than other vaccine providers which is the first step in creating lasting and efficient changes within the system. That being said, there is still a lack of data which makes it difficult to confirm how much equity is really being solved during the pandemic, as emphasized previously, but many opportunities exist for FQHCs to improve their outreach and the process doesn’t happen overnight. Seeing as there is still a large amount of the U.S. population that hasn’t been vaccinated yet, there will hopefully be more data released as distribution advances which will ultimately help FQHCs to further develop such equity on a larger scale, and permanently.




