Value-based care is quickly moving from “talked about” to “reality” in healthcare. As providers are implementing new value-based arrangements, there are a lot of issues that are coming to light that may not have been fully thought out or realized before.
Stakeholders from across the healthcare ecosystem discussed several of these realities recently at Xtelligent Media’s Value-Based Care Summit, held in Boston. While I have a notebook filled with takeaways from the event, here are a few themes that stood out on what providers need to be cognizant of as we move to a more value-based world.
1. There’s an overload of data, but a dearth of information
Nearly all of the presentations at the summit talked about data in some capacity. And the sentiment was generally the same all around. There is a lot of data available in healthcare—too much data, many would say—but there is not a tremendous amount of insight being generated from that data.
Some of the problems that prevent those in healthcare from making data-driven decisions:
- Lack of trust in the data. In his keynote at the summit, Tom Skelton, CIO of SureScripts talked about the importance of information sharing, saying it is the “root system” (like the roots of a tree) that we need in healthcare. Unfortunately, information is not moving as it should because there is a deficit of trust both between providers and between technology providers.
- Lack of interoperability. Interoperability is still a hot-button topic in healthcare, as I wrote about recently. As we move to a value-based system, it’s really important that providers understand the history and context of a patient, and that means having access to all medical records, not just those within the four walls of the hospital. Even within hospitals, it can be hard to exchange information between departments. For example, one provider talked about how the hospital could “see” patient data from another department, but this information was not integrated into the patient record.
- Integration into the workflow. Many healthcare providers have a difficult enough time getting clinical staff to use an EHR. Now they should be expected to learn additional technology? Fact is, if it does not fit into their daily workflow, it’s going to be really difficult to get providers to use new technology. Physicians and nurses are already overworked. They are not likely to learn something new.
2. Social determinants of health are really important
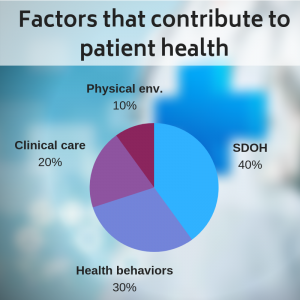 At the event, Dr. Alisahah Cole of Atrium Health in North Carolina delivered an excellent presentation titled, “Integrating Social Determinants of Health into Patient Management.” Social determinants of health (SDOH) include things like the availability of fresh food, transportation options, quality of education, exposure to crime and violence, and so on. Dr. Cole presented statistics that show that:
At the event, Dr. Alisahah Cole of Atrium Health in North Carolina delivered an excellent presentation titled, “Integrating Social Determinants of Health into Patient Management.” Social determinants of health (SDOH) include things like the availability of fresh food, transportation options, quality of education, exposure to crime and violence, and so on. Dr. Cole presented statistics that show that:
- 40% of one’s health is determined by social determinants of health
- 30% is determined by one’s health behaviors
- 20% is determined by clinical care that one receives
- 10% is determined by one’s physical environment
How are healthcare providers expected to make improvements in patient health—that are necessary for compensation—when so much of it is beyond the providers’ control? According to Dr. Cole, new technologies such as telehealth and virtual behavioral health options are valuable here and have been demonstrated to improve patient outcomes. In addition, some providers are thinking differently—for example, by partnering with food banks to offer fresh food. By reaching out to patients in new ways and by partnering with others in the community, providers can move the needle on patient outcomes.
3. Where patients get care is changing… and it will impact the way healthcare is delivered
As we move toward value-based care, there will also be a shift in where patients receive care. Several panelists at the summit spoke of how care will be shifting away from the hospitals and closer to the patient. For example, Partners Healthcare in the Boston area is anticipating larger investments in ambulatory centers in the coming years. We have also seen increases in the number of microhospitals as well as telemedicine options.
What this means for providers is that they will need better integration between their hospitals and their physicians out in the field, as noted above. It also means they will need access to data and analytics that can help them make better clinical decisions to treat their patients out in the field.
Moving forward
It’s clear that the road to value-based care isn’t without its twists and turns. There are several challenges that healthcare providers need to carefully consider as payment models change and they become more accountable for patient outcomes. Technology providers need to consider these challenges as well and provide solutions that enable more integrated, faster, and improved care for patients.
Read more
- Collaborative Data Governance Fosters Reliable Analytics and Organizational Improvements
- The Single Source of Truth: Measure Factory Revolutionizing Data Analytics for Healthcare
- Solving Hospital CEOs’ Pressing Challenges With Analytics - April 15, 2024
- Navigating the Wellness Wave: Wine & Spirits Data Strategy - April 9, 2024
- Takeaways from HIMSS24 - March 26, 2024



